SSRI Teeth Grinding (Bruxism): Causes, Fixes & Safe Relief

You started an antidepressant to feel steadier, and now your jaw feels like it worked a night shift. Morning stiffness, tender cheeks, tight temples, maybe a partner complaining about scraping noises at 2 a.m.—that cluster points to SSRI teeth grinding (also called SSRI bruxism). It’s not rare, it’s not your fault, and it doesn’t mean you have to choose between mental health and a healthy jaw. You just need a clear plan.
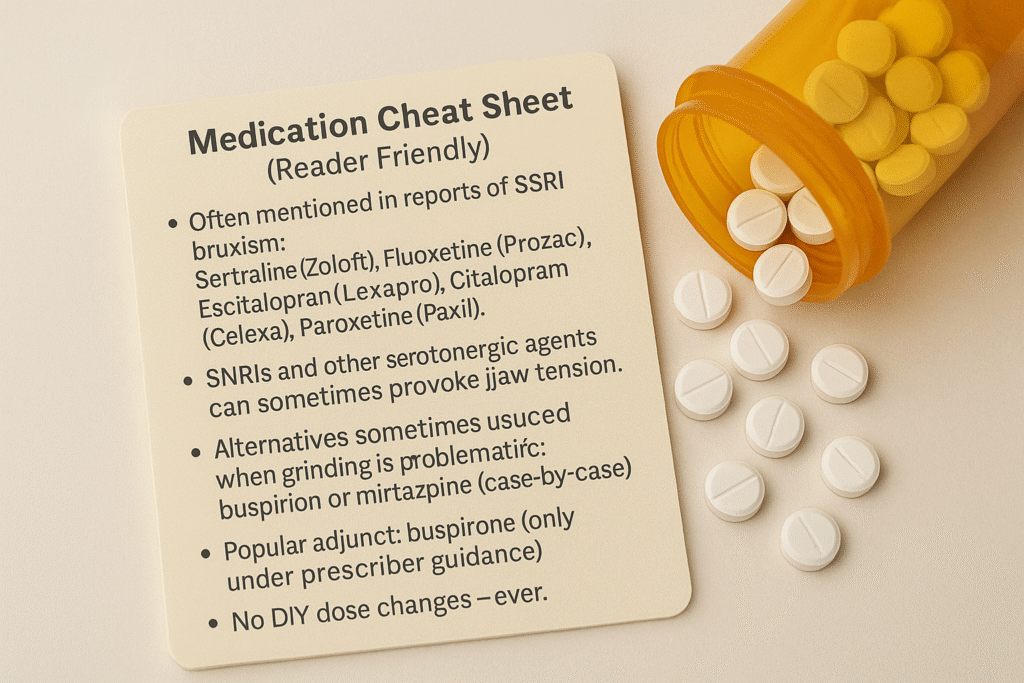
- Can SSRIs cause bruxism or jaw clenching? Yes—some people develop antidepressant jaw clenching within days or weeks of starting or increasing an SSRI (sertraline, fluoxetine, escitalopram, citalopram, paroxetine).
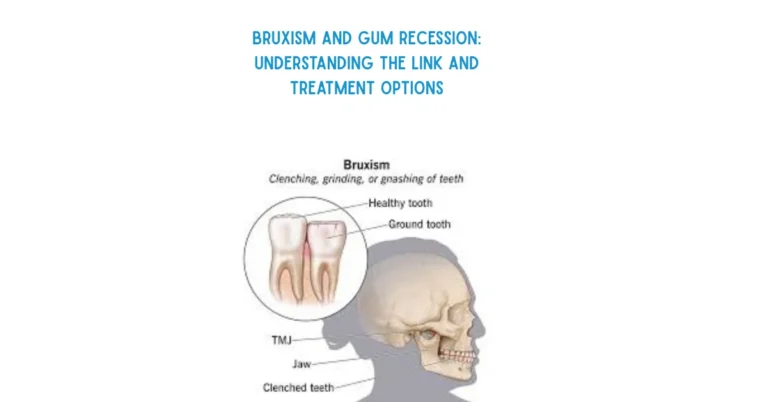
- What does it feel like? Night grinding, daytime clenching, temple headaches, sore masseter muscles, tooth sensitivity, and sometimes clicking or ache in the TMJ.
- What fixes it? Protect teeth (a night guard for bruxism), reduce afternoon caffeine, practice jaw-relax habits, and—crucially—work with your prescriber on dose timing/adjustment, adding buspirone for SSRI bruxism, or switching to another antidepressant (e.g., bupropion or mirtazapine) when appropriate.
- Important safety note: Don’t stop SSRIs abruptly; changes must be guided by your clinician.
What SSRI-Related Bruxism Looks Like in Real Life
Daytime clues
- You notice your teeth touching hard when you’re driving, gaming, or deep in emails.
- Your jaw sits slightly forward, lips pressed, shoulders up.
- You catch yourself “micro-clenching” during stress, then feel a wave of fatigue across your cheeks.
Nighttime pattern
- A partner hears grinding; you wake with tightness along the jawline and a dull ache near the ears.
- Teeth feel sensitive to cold. Edges look flatter than they used to.
- Headaches cluster around the temples or behind the eyes.
Red flags (call a dentist/doctor promptly)
- Jaw locking open or closed, swelling near the joint, a tooth fracture or a crown that suddenly feels wrong, or jaw pain paired with chest pain/shortness of breath (seek urgent care for that last one).
Why SSRIs Can Trigger Teeth Grinding?
SSRIs raise serotonin to help mood and anxiety. Serotonin also talks to dopamine, which helps smooth and coordinate movement. In a subset of people, more serotonin can dampen dopamine tone in motor circuits. Think of dopamine as the road’s shock absorber; when it’s dialed down, small bumps feel big. The jaw—one of the body’s strongest, most reflexive muscle groups—responds with clenching or grinding.
This doesn’t happen to everyone. Risk is influenced by dose, how quickly you titrated, your unique brain chemistry, other meds (including SNRIs or stimulants), caffeine/nicotine, and sleep quality.

How Soon It Starts and How Long It Lasts?
- Onset window: commonly days to weeks after starting an SSRI or increasing the dose. People often report “I was fine, then after the bump from 50 to 100 mg… my jaw went crazy.”
- Course: symptoms often peak at night and show up as morning soreness or partner-reported grinding.
- Resolution: with the right plan—guard + lifestyle tweaks + prescriber changes (dose timing, dose reduction, buspirone, or switch)—many notice improvement in days to a few weeks. Dental and muscle tissues may take longer to fully calm.
Rule-Outs and Look-Alikes
Before blaming the pill bottle, check for other drivers:
- Pre-existing bruxism from anxiety or stress: was the grinding there before medication? If so, improvement in mood might actually help.
- Caffeine or stimulants: afternoon coffee, energy drinks, or ADHD stimulants can amplify clenching.
- Sleep apnea or fragmented sleep: snoring, gasping, or significant daytime sleepiness suggests airway-driven bruxism.
- TMJ disorders unrelated to meds: disc displacement or joint inflammation can cause clicking/locking and pain.
- Nicotine and dehydration: both heighten arousal, nudging the jaw toward tension.
A symptom diary for 10–14 days helps: track dose and time, caffeine and alcohol, sleep quality, stress spikes, and jaw symptoms (0–10). Patterns become obvious fast.
The Stepwise Plan That Works
You’ll coordinate two lanes: prescriber lane (medication plan) and dental lane (protect and repair). Start both this week.
Lane 1 — Protect teeth and calm the jaw (start today)
- Custom Teeth night guard for bruxism: get one from your dentist. It doesn’t stop the brain from initiating grinding, but it prevents enamel wear and reduces TMJ load immediately.
- Caffeine cutoff by early afternoon: serotonin–dopamine balance aside, caffeine late in the day fragments sleep and spikes clenching.
- Jaw-reset drill (60 seconds): tongue resting gently on the palate behind the front teeth; lips together; teeth apart; inhale 4, exhale 6; repeat 6–8 cycles. Do it at red lights, between emails, and before bed.
- Warmth for muscles: a heat pack on cheeks and temples for 10 minutes before sleep; muscles release when warm.
- Micro-breaks for screens: every 45 minutes, drop your shoulders, unclench, and look far away for 20 seconds.
- Hydration + steady meals: dehydration and blood sugar dips both increase muscle tension.
Lane 2 — Talk to your prescriber (don’t change meds alone)
Go to the appointment with your diary and ask about these medically guided options:
- Dose timing or slight dose reduction
- Moving the dose earlier or easing to the lowest effective dose can reduce nighttime jaw over-activity for some people.
- Buspirone for SSRI bruxism
- Frequently used as an adjunct to rebalance neurotransmission. Many patients report improvement within days to two weeks.
- Switching antidepressants
- When grinding is severe or persistent, a move away from the triggering SSRI may be considered. Common destinations: bupropion (more dopamine/norepinephrine) or mirtazapine (different receptor profile). The choice depends on your mental-health history and side-effect tolerability.
- Short-term add-ons
- In selected cases and under supervision, a brief course of a muscle-relaxing or anxiolytic medication can be used while other adjustments take effect. This is not a long-term solution for most.
Lane 3 — Dental follow-through
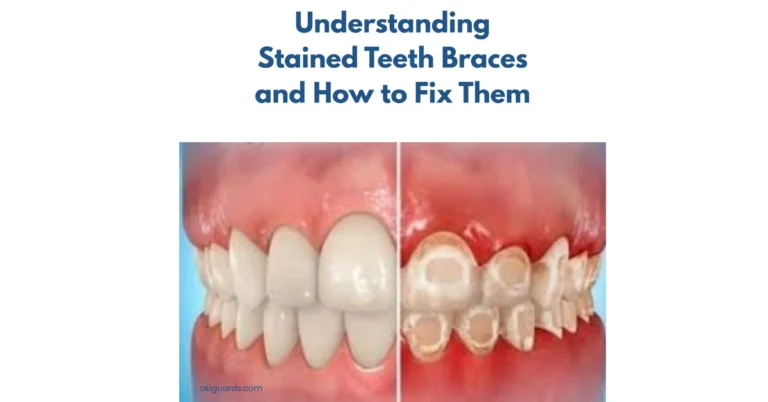
- Wear check: your dentist looks for fresh wear facets, enamel micro-chips, and irritated gums.
- Guard fit adjustments: a well-fitted guard spreads force evenly and preserves restorations.
- Sensitivity care: desensitizing varnish or bonding for exposed dentin if needed.
- TMJ support: referral to physical therapy or a myofascial specialist if joint or muscle pain lingers.
How You’ll Know the Plan Is Working
Week 1
- Start guard; move caffeine to mornings; do heat + jaw-reset.
- Expect slightly less morning tightness and fewer temple headaches.
Week 2
- After prescriber changes (e.g., buspirone or dose timing), episodes often thin out. You might still clench during a stressful meeting, but the nights begin to quiet.
Weeks 3–4
- Masseters feel less pumped; tooth sensitivity eases; partner hears less grinding. Guard feels natural. Energy improves as sleep stabilizes.
Weeks 5–8
- If the plan is right, you settle into a comfortable baseline. If not, revisit with your prescriber about a switch or a different adjunct.

Practical Home Support
- Evening wind-down: dim lights, phone away, brief breathing or gentle stretching.
- Magnesium-rich foods: leafy greens, legumes, nuts, seeds; discuss supplements with your clinician first.
- Alcohol and nicotine: both fragment sleep and raise arousal; cutting back helps the jaw stay quiet.
- Posture and ergonomics: lift screens to eye height; keep elbows supported; unlearn “tech-neck” that tightens the jaw chain.
Myth-Buster Lightning Round
- Myth: “Only anxiety causes grinding.”
Fact: Medication effects, stimulants, nicotine, and sleep disorders can drive it—even when anxiety is well controlled. - Myth: “A guard fixes the problem.”
Fact: The guard protects teeth and joints; the medication plan fixes the driver. - Myth: “Side effects always fade if you wait.”
Fact: Sometimes they do, sometimes they don’t. If your teeth are at risk, waiting isn’t wise—adjust with your clinician. - Myth: “All SSRIs will do this to me.”
- Fact: Responses are individual. Some people never develop bruxism; others do on one SSRI but not another.
FAQs: Side Effects of SSRI Teeth Grinding
How to stop grinding teeth on antidepressants
Protect with a night guard, cut afternoon caffeine, add heat and a jaw-reset habit, and ask your prescriber about dose timing/adjustment, buspirone, or a switch (e.g., bupropion or mirtazapine) if needed.
Zoloft teeth grinding vs. Prozac teeth grinding vs. Lexapro bruxism
All three can trigger bruxism in some people. Which one does for you—and at what dose—depends on personal brain chemistry. Track symptoms and work with your prescriber.
Is SSRI bruxism permanent?
No. With the right plan, symptoms typically resolve. Guard your teeth while changes take effect.
What exactly is SSRI bruxism?
It’s teeth grinding or jaw clenching that begins after starting or increasing an SSRI. It can happen during the day, at night, or both.
Which antidepressants are least likely to cause grinding?
It’s individualized, but bupropion and mirtazapine are commonly discussed alternatives when SSRI bruxism is problematic. Your clinician will weigh benefits and side effects for you.
Can buspirone really help SSRI bruxism?
Many patients do improve when buspirone is added to an SSRI regimen under medical supervision. Some notice change within days to two weeks.
Will a night guard stop the grinding itself?
A night guard doesn’t stop the brain from initiating grinding; it protects teeth and reduces TMJ strain while the medication plan is optimized.
Could SNRIs or other meds cause similar clenching?
Yes, any agent that shifts serotonin/dopamine balance might. That’s why timing and a symptom diary are so useful.
Is it safe to alter my SSRI dose by myself?
No. Abrupt changes can cause withdrawal or relapse. Always change meds with your prescriber.
Can Botox help if my jaw muscles are overactive?
In select, stubborn cases, masseter Botox may reduce muscle force for a few months. It’s a specialist option—discuss risks/benefits with your clinicians.
How do I protect my teeth while we sort the meds out?
Wear a custom night guard, keep caffeine earlier in the day, use a fluoride toothpaste for sensitivity, and avoid chewing ice or very hard foods.
Does grinding mean my SSRI isn’t right for me?
Not necessarily. Some people stay on the same SSRI with a dose tweak or buspirone and do great. Others feel better after a switch. The best plan is the one that protects your mental health and your teeth.
When should I see a dentist urgently?
If you suspect a cracked tooth, your bite suddenly feels off, your jaw locks or swells, or pain is severe and constant.