Gum Recession: Causes, Treatment, and Plan That Actually Works
Your teeth didn’t suddenly grow overnight—your gums stepped back. That’s what gum recession is: the gumline creeps downward (upper teeth) or upward (lower teeth) so more tooth and root show. It can feel scary, but you’re not powerless. With the right steps you can stop it from getting worse and, when appropriate, restore protection and coverage.
- Can gums grow back naturally? No—once gum tissue is lost, it does not regrow on its own.
- Can the situation be fixed? Yes—by controlling causes, improving daily care, and, if needed, using procedures that restore coverage and thicken tissue.
- First move: get an accurate diagnosis so you know whether the main driver is gum disease, aggressive brushing, thin tissue, bruxism (grinding), a misaligned bite, tobacco, or something else.
Spotting Gum Recession Early
What it looks like
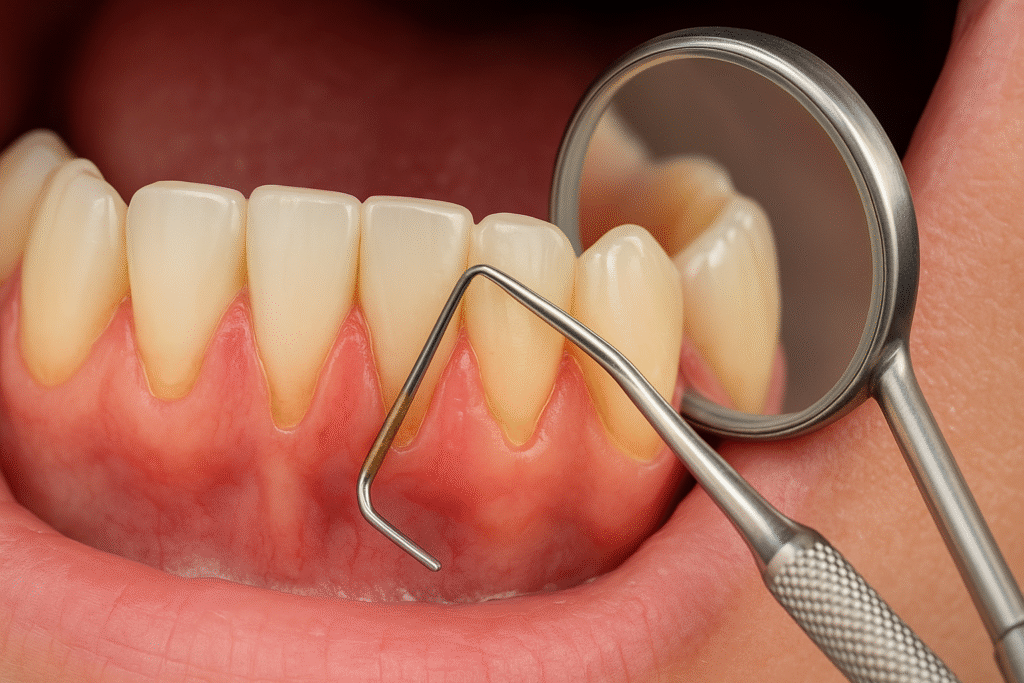
- Teeth look longer than before
- You can see a notch or groove near the gumline
- Exposed roots (darker/yellower near the neck of the tooth)
- Tooth sensitivity to cold air, sweets, or touch
- Gums look thin or uneven; food traps appear where none existed
What needs urgent attention
- Gum or facial swelling, pus, fever
- Sudden tooth mobility or a bite that feels “off”
- Pain that wakes you up or isn’t helped by over-the-counter relief

Why Receding Gums Happen (and Which Causes You Can Control)
Think of recession as a team effort between biology and behavior. Often more than one factor is involved.
Periodontal disease (gingivitis → periodontitis)
Plaque and tartar irritate gums; they bleed, swell, and, if the condition progresses, bone support around teeth can shrink. As support recedes, the gumline follows.
Aggressive brushing or the wrong brush
“Scrub harder” is the villain here. Stiff bristles or heavy pressure can physically wear gum edges and the enamel/cementum at the neck of the tooth.
Thin biotype and genetics
Some people naturally have a delicate gum “biotype.” Movement of teeth outside the bony envelope (past orthodontics or natural drift) plus thin tissue equals a higher recession risk.
Misaligned teeth and occlusal load
Crowding, flared teeth, or an uneven bite put concentrated force on certain gum margins. Over time those edges can retreat.
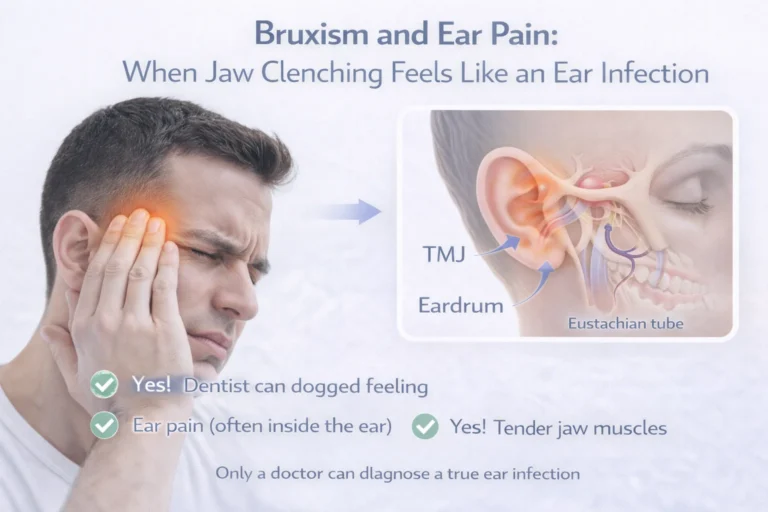
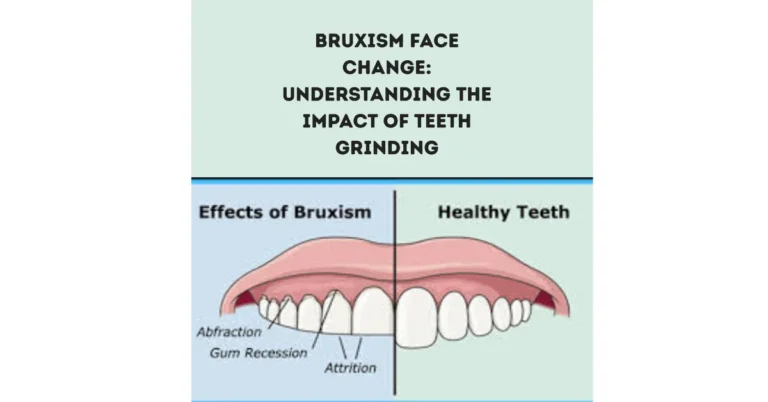
Bruxism (grinding and clenching)
Excessive nighttime force doesn’t always start recession, but it can worsen it. A night teeth guard reduces trauma while you address other causes.
Tobacco/vaping and systemic factors
Nicotine restricts blood flow and slows healing. Uncontrolled diabetes, certain medications, and life stages (pregnancy, menopause) can also change how gums respond.
Piercings and repeated friction
Lip or tongue jewelry bumping against the gum is a mechanical irritant. Over years, it’s like sandpaper.

Reverse vs. Restore—Two Different Goals
A lot of confusion comes from mixing two ideas:
Reverse gingivitis: swollen, bleeding gums can return to health with professional cleaning and great home care.
Restore recession: lost gum coverage doesn’t come back naturally; dentists use specific methods to restore protection and appearance (thicker tissue, covered roots).
So the playbook is: stabilize health → reduce forces and irritation → restore where needed.
How Dentists Diagnose Gum Recession (So You Don’t Guess)

What the exam includes
- Periodontal charting: measuring pocket depths at six points per tooth
- Recession mapping: how far the gum edge has moved
- Plaque/tartar mapping: where irritants live
- Bite/force check: which teeth take the hit first
- Sensitivity tests & X-rays: root exposure and bone levels
This map determines the order of treatment—what to fix first, and which sites (if any) need surgical coverage.
The Treatment Ladder (Foundations First, Then Fixes)
You build results like a house: strong foundation, then structure, then finish.
Step 1 — Daily habits that protect (the foundation)
- Soft-bristled toothbrush only. Hold at a 45° angle to the gumline; use small circles with light pressure.
- Interdental cleaning daily (floss or interdental brushes—whichever you’ll actually use).
- Fluoride toothpaste for sensitive exposed roots; let it sit (don’t rinse right away).
- Quit tobacco/vaping if you can; gums heal better and stay healthier.
- Replace brushes/heads every 1–3 months or sooner if frayed.
Step 2 — Professional cleaning and disease control
- Routine cleaning if buildup is mild.
- Scaling and root planing (deep cleaning) if there’s periodontitis: cleans below the gumline and smooths root surfaces so tissue can calm and reattach.
- Antimicrobial therapy (rinses or localized medications) may be used short-term where bacterial load is high.
Step 3 — Balance the forces
- Teeth Night guard for bruxism: spreads forces, protects edges while other work heals.
- Bite adjustment if certain teeth hit too hard or first.
- Orthodontics if tooth position outside bone is fueling recession—aligners or braces can bring teeth back into a safer, more stable zone.
Step 4 — Restore coverage and thicken thin tissue
When roots are exposed, sensitivity lingers, or tissue is too thin to resist future loss, your periodontist may recommend one of the following:
- Connective tissue graft (CTG): Palatal (or donor) connective tissue is placed under a flap to thicken and cover recession—often the gold standard in many sites.
- Free gingival graft (FGG): Adds a band of tougher, keratinized gum (great where you need more protective tissue, often in lower front teeth).
- Pedicle/tunnel techniques: Repositioning adjacent tissue to cover the recession with minimal surface incisions; often used for multiple neighboring teeth.
- Biologics or substitutes: In selected cases, graft substitutes or biologic agents support healing and thickness.
- Bonding/desensitizers: For small, stable areas (or as an interim step), bonding can cover sensitive root dentin and smooth plaque-catching notches.
The aim isn’t just looks—it’s durable thickness that resists future trauma, with roots protected under a healthy, stable gumline.
What Recovery Actually Feels Like (Week by Week)
Every mouth heals a bit differently, but most patients recognize this timeline:
Days 1–3
- Mild swelling/tenderness; soft foods; avoid brushing directly over the site
- Use the rinse and meds your clinician provides; sleep with head slightly elevated
Days 4–7
- Tenderness fades; you’ll be careful not to tug your lip to “peek” at the site
- Sensitivity usually begins to settle
Around 1–2 weeks
- Sutures are often removed; talking and eating feel mostly normal again
- Gentle brushing is reintroduced as advised
Weeks 3–6
- Tissue matures and blends in; follow-up focuses on technique, pocket depth stability, and bite forces
After 6 weeks
- Most activities are fully normal; you’ll keep your maintenance schedule to protect the result long-term
The Daily Playbook to Stop Recession From Getting Worse
Technique over force
- Soft bristles + light pressure + small circles = clean without damage
- Consider an electric brush with a pressure sensor if you tend to scrub
Clean the spaces
- Floss, floss picks, or interdental cleaning brushes—pick the tool you’ll use daily
Fluoride is your friend
- Sensitive roots respond well to fluoride; don’t rinse right after brushing so fluoride can linger
Control the stress on gums
- If you grind, wear the night guard consistently
- Ask your dentist about small bite refinements if you hit hard in one spot
Remove friction
- If lip/tongue jewelry rubs the gumline, consider removing or changing it
Health basics
- Tobacco cessation, steady blood sugar if you’re diabetic, and routine checkups all improve gum stability
When to See a Periodontist (Specialist) Right Away
- Exposed roots with ongoing sensitivity despite careful home care
- Thin tissue that continues to recede or tear
- Pocket depth that stays deep after cleaning, or tooth mobility
- Recession in the smile zone you want corrected aesthetically
- Complex drivers (misalignment + grinding + thin tissue) where a coordinated plan is best

Cost Factors (Why Prices Differ)
- Number of teeth and technique used
- Whether donor tissue (your palate) or a graft substitute is chosen
- Site complexity (thin tissue, root anatomy, location)
- Geographic region and clinician expertise
- Additional care (deep cleaning, night guard, orthodontics)
Myth-Buster Lightning Round
- “Receding gums grow back with oils or vitamins.”
No topical or supplement regrows gum tissue. Good hygiene and professional care stop progression; grafting restores coverage. - “Hard bristles clean better.”
They clean faster—and carve faster. Use soft bristles; let the bristles do the work, not your shoulder. - “Mouthwash replaces flossing.”
Rinses help, but they don’t push plaque out of the tight spaces. You still need floss or interdental tools. - “If it isn’t painful, it isn’t serious.”
Recession can be quiet for years while roots wear and bone support thins. Don’t wait for pain. - “Braces cause recession.”
- Poorly planned movement can, yes. Thoughtful orthodontics that keeps teeth within bone—with great hygiene—protects gums.
Frequently Asked Questions
Can receding gums grow back naturally?
No. Receding gums do not grow back on their own. You can halt progression with professional care and daily habits, and you can restore coverage with gum graft surgery when needed.
What causes receding gums?
Common drivers include periodontal disease, aggressive brushing or hard bristles, thin gum tissue (genetics), misaligned bite, bruxism (grinding), tobacco/vaping, and rubbing from oral piercings.
How do dentists treat gum recession?
Start with health: professional cleanings and scaling and root planing if disease is present. Reduce forces (night guard, bite balance, orthodontics). When roots need protection or tissue is too thin, use grafting procedures—connective tissue graft, free gingival graft, or pedicle graft/tunnel techniques—to restore thickness and coverage.
Is gum graft surgery painful?
You’ll be numb during the procedure. Most people report soreness rather than sharp pain afterward. A soft diet and careful hygiene near the site are typical for the first week.
How long is recovery after gum graft surgery?
Expect mild swelling for a few days, suture removal around 1–2 weeks, and steady comfort gains over 3–6 weeks as tissue matures. Your team will tailor instructions to your case.
Can I fix recession without surgery?
You can stop it getting worse with gentle technique, professional care, fluoride, and force control (night guard). For durable tissue thickness and root coverage, a graft is the predictable option.
Which toothbrush should I use?
A soft-bristled toothbrush (manual or electric) with light pressure. The secret is the motion: small circles at the gumline—no hard scrubbing.
Does grinding really make it worse?
Grinding can exacerbate recession by adding force to already thin or inflamed tissue. A Teeth night guard lessens trauma while you address disease and technique.
Will mouthwash help?
It can support gum health, but it doesn’t replace flossing or interdental cleaning. Think of it as a helper, not a substitute.
How do I keep results long-term?
Gentle daily care, fluoride, regular cleanings, tobacco cessation, force control (guard/bite balance), and follow-ups with your dentist or periodontist. That routine protects your investment.

The Bottom Line
Gum recession isn’t a life sentence—and it isn’t a DIY project either. Get a clear diagnosis, fix the drivers (disease, technique, forces), and then choose the right procedure if you need restored coverage. Combine soft-bristle brushing, interdental cleaning, fluoride, a Teeth night guard if you grind, and regular visits, and you’ll protect your roots, your comfort, and your smile for the long run.
You don’t have to watch your gums slowly step back. With the right plan—and a little patience—you can stop the slide and build a healthier, stronger foundation.